Backpain is one of the leading causes of disability world wide. It also does not discriminate, it can occur in all age groups.
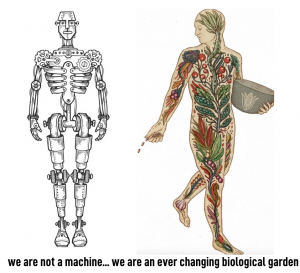
There are types of back pain that are normal for us to experience (90-95% of cases) these are labelled ‘non-specific’ meaning there is no immediate threat to your survival even though it can feel quite painful and stop you from doing things.
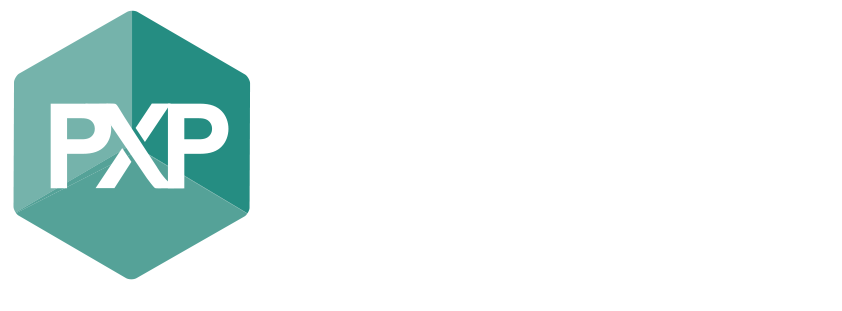
Then there is back pain that may have ‘red flag’ factors and are considered ‘specific’ causes (5% of cases) of pain where there may be a threat to your health and survival and further medical investigation is warranted.
The Unhelpful…
Scans – MRI, Xray, CT, Ultrasound…
Most people who present to our clinic with back pain – ask the question: “Should I get a scan?”
Others come in with having already seen another health professional along with a referral for a scan and bring in a report of the scan’s findings.
Let’s be honest, the wording in a radiology report is not easy to read and if you don’t have a good understanding of the terminology it can sound pretty bad, when in actual fact it most probably isn’t.
A radiology report is a description of the anatomy and what is looks like in picture format however the description does not take into consideration ‘normal’ tissue changes nor does it tell us exactly where the pain is.
The issue is when a patient has the expectation that the scan is going to tell them what is wrong with them and what could be done to fix it.
However 90-95% of the time the scan is mostly unhelpful and unnecessary.
We have then this silent belief developed by the patient (not their fault) from the health professional’s (unconsciously at fault) referral for scan that they must know what their tissues are like (muscles, bone, ligaments etc) for them to improve their pain. This is just not the case in most situations.
There is and has been for a long time an over servicing for scans by health professionals. It is getting better as the evidence and particular necessity for scans is being practiced.
However, it is something that has been taken for granted and we thought scans gave us all the information we needed to assist in treatment.
This also leads us to over diagnosing you. Health professionals have been using complex treatments to treat something that is nothing but simple. We most often have been creating situations where people are believing that their back is for some what of a better word “stuffed”.
Of course health professionals want to help, it is what we do and we do anything in our belief to help you. However our beliefs can sometimes be unhelpful to you without us knowing it.
A picture of your bones/muscles/nerves etc creates fear and can lead to what someone has to live by. How many times have you heard a friend say I have a ‘bulging disc, or ‘my spine is degenerating’.
A scan’s result can even create fear within the practitioner and so avoidance of evidence based practice is well… avoided.
These terms are not necessarily what is happening for that person at that moment. These things heal and adapt and get better, changes happen slowly over time with or without pain. We are a biological system that grows, however we get stuck in our beliefs of what our structure is doing much like a piece of a machinery.
We are not mechanical robots, we are basically just like a walking garden that adapts to its environment when necessary. When you think of us that way… it’s pretty cool.
When you put it in perspective this type of unhelpful practice has stopped grandparents picking up their grandchildren, gardeners letting their gardens overgrow or golfers quitting the game in their prime. In the younger cohort we have tradesman unable to get back to work due to fear of re-injury and athletes who have quit a sport they love. On top of this there is a massive knock on effect.
We share our experiences with our lovedones as a way to protect them because of what we think we know or have learnt so we teach the next generation the ‘bad’ things to come further igniting poor belief’s.
The helpful….
What does the evidence say?
It is uncanny how strong our tissues are, they cope with high repetitive demands and loads for a lifetime and we have a biological system that adapts to the stimulus that it is exposed to this happens throughout our life. We are super strong and that is without any additional strength program. It is what it is.
For nearly all people with back pain 90-95% when there are no characteristic red flags their pain is labelled ‘non specific’.
The typical list of conditions that fit this description are things that you may have heard before. Disc herniation, scoliosis, spondylithesis, disc degeneration, facet joint degeneration, osteoarthritis.
The term “non specific” is a very annoying term to frankly, come to terms with!
Basically, our body tissues (bone, muscle etc) change all through our life with or without pain and this is considered ‘normal’. It has more to do with how we use our body (or don’t use it) and what our body will do to adapt to it’s environment. All for a good cause of course – staying alive.
So if I have ‘non-specific’ back pain which is basically ‘normal’ why is my pain so bad?
Well it’s complicated…
I think it is important to understand pain and what pain is – in a nut shell – pain does not equal damage to your tissues it is merely a warning signal like an alarm bell.
Our nervous system is build to protect us and sometimes in certain people and in certain situations it can be a very powerful communicator of danger or threat (ie. pain) when in actual fact there may not be any danger at all.
The intensity and frequency of this pain response is a concoction in our neural synapses that have analysed ‘threats’ to you all your life. Our nervous system develops a type of ‘signature’ of what it believes to be things that could potentially ‘harm us and things that are ‘safe’ to us. It is completely a clever, individualised, multifactorial system.
Of course things that actually threaten us for real (being in a major car accident or having a major trauma) doesn’t usually hurt at the time because our nervous system needs to help us survive. There is no need to warn you, you need enough power to get out of there and get help. Most people who get help then get pain after because you know you will be ok but the alarm (pain) is there to remind you.
It’s the same reason why a toddler who’s fallen looks for their parents and once they see their parents they cry.
In persistent long term pain that warning system can have a larger warning buffer and happen at much lower states of threat and this is to do with long term potentiation (learning from our neural system which helps create our signature of protection so we get pain when there is no need for us to be protected by it. In simple terms we can learn to have pain – practice makes perfect.
Then if you add in if you are stressed, sick, overwhelmed, anxious, hungry, tired and sedentary you are more likely to get that message of threat…. PAIN.
So if you are one of many who have seen a health professional who has not reviewed all of the above factors that could be involved in your pain experience and instead sends you for an unnecessary scan which have then been sent for an unnecessary appointment with a surgeon or specialist and in same cases has unnecessary surgery.
We are concreting our nervous system’s belief that there are more and more threats. Many cases of surgical interventions for back pain do not result in reductions of pain when the expectation is that it will (especially in the ‘non specific 90-95% group).
Even current modes of pain relief using medications such as opoids or morphine can assist in growing our ability to learn pain. Rather than challenging a system that believes there is threat when there isn’t, we hide it and so it has a solid ground to learn from. Doesn’t make sense does it?
The helpful going forward…
So what can we do about it? Back pain is not comfortable, it’s a very unpleasant experience….
Recently sys
tematic reviews from world leading researchers have put together new ongoing guidelines on how we should be approaching the treatment of back pain as per the overwhelming evidence. These look at common, most widely sourced treatments and their effectiveness and then gave recommendations on the new guidelines going forward.
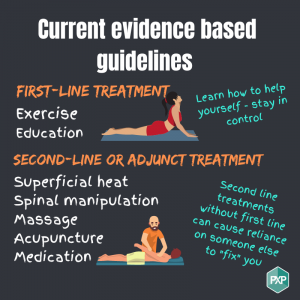
In the guidelines they report on what are and should be the first line of treatment for back pain and then second line of treatment or adjunct treatment.
First line of treatment are: Exercise, education on pain, learn how you can help yourself
Second line of treatment are: Superficial heat, spinal manipulation, massage, acupuncture, medications
However most of us for decades just use second line treatments and skip first line treatments all together or spend more time in second line treatments until they feel their pain is better enough to start first line treatment. Doing this can result in strengthening beliefs that something is not right, avoidance of many activities and adding to the self unconscious belief that there is something wrong which can increase that persons threat.
But don’t forget…
The other 5-10% of back pain suffers are from ‘specific’ causes. These are the important rare red flag situations that health professionals are screening for. They will put you through a battery of questions and tests to make sure you do not fit into this category. If you do further testing may be requested. All allied health and general practitioners should be skilled in recognising these. This is what we screen for and why we ask many questions when you visit us.
Specific back pain includes those that are at high risk of further medical issues such as infection, osteoporosis, fractures due to trauma, severe neurological symptoms, cancer, autoimmune diseases. 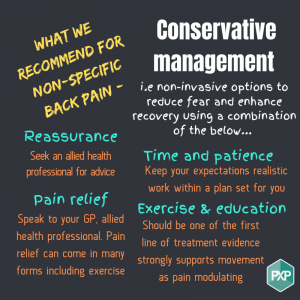
In these situations it is warranted that you may need a scan, blood test and/or specialist assistance.
So the answer to the original questions is 90-95% of the time you do not need a scan however you may need some assistance to feel better because pain is an unpleasant experience and it could be stopping you from doing many things.
Movement and exercise is the key and first line of treatment as well as education on what pain is and why you may be experiencing it. You may also decide you would like to do second line treatments or adjust therapies as well to assist in recovery however we recommend not waiting or avoiding movement.
Not sure what movement you can do, that’s where a clinical exercise professional like an Exercise Physiologist or Physiotherapist can assess your movement and prescribed the right programming for you. The goal should be to help you help yourself and stay in control!
Finding the right professional who is following the evidence is important.
If you see a second line treatment provider and they recommend you move and exercise you’re seeing the right person because they know the large benefits of doing so and have your best interests at heart.
If your doctor or allied health professional has not advised you about exercise, ask them about it, question them and then make up your own mind.
Hopefully this article has assisted you to recognise that back pain is a normal part of life and most episodes are not serious and don’t need any formal treatment. Knowing more than you need to can be unhelpful and encourage your pain to continue.
Low back pain is a complex condition caused by a multitude of factors, both mechanical, environmental, and psychological, but just because its complex it doesn’t mean its management needs to be complicated.
Written by: Beth Chiuchiarelli AEP, AES