What is Osteoporosis?
Osteoporosis is a decline of bone mineral density (BMD), which is the strength and thickness of our bones. This decline increases an individual’s susceptibility to fracture. The most common locations osteoporosis presents are the spine, pelvis, wrists and forearms. Another term used for a decline in bone density is Osteopenia. In Australia, 6% of men and 23% of women over 50 have osteoporosis. As age increases over 70 the prevalence of osteoporosis also increases to 13% of men and 43% of women.
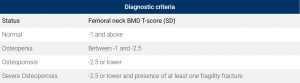
What is the diagnostic criteria for Osteoporosis and Osteopenia?
A DEXA scan is the gold standard for testing and measuring for osteoporosis and osteopenia. The machine (DEXA) scans different areas of your body to assess the density of the bone. The typical locations are the neck of the femur and lumbar spine. The score is calculated from how many standard deviations the individual’s bone mass is from peak bone mass of a young adult. A T score greater than -2.5 is diagnosed as osteoporosis. Osteopenia is a low BMD where the person is at risk of developing osteoporosis and has a T score of -1 to -2.4.
The good news is that bone has the capacity to adapt and change through loading.
Therefore, individuals with osteoporosis or osteopenia can complete exercise to prevent further decline. Risk factors that contribute to the decline or the risk of developing osteoporosis can be either modifiable or non-modifiable. Modifiable is something you can change and non-modifiable or fixed risk factor is something you were either born with or can’t change.
Modifiable risk factors include:
- Sedentary lifestyle/ Physical inactivity
- Alcohol consumption
- Smoking
- Poor nutrition
- Vitamin D deficiency
Fixed/ Non modifiable risk factors:
- Age >50
- Female
- Family history
- Hormonal changes in particular menopause
- Previous fracture
- Ethnicity
As highlighted above, one of the modifiable risk factors is physical inactivity/sedentary lifestyle. This means that individuals who are not active have an increased risk of developing Osteoporosis as they are not loading their bones enough.![]()
How can exercise help?
Exercise is “osteogenic in nature” meaning it helps produce new layers of bone and prevent the decrease in bone density. Exercise also helps to increase muscle mass and improve balance and coordination assisting in the prevention of falls. Falls are one of the most common causes of fracture so through preventing falls the risk of fracture is likely decreased.
Myths and concerns surrounding exercising with osteoporosis.
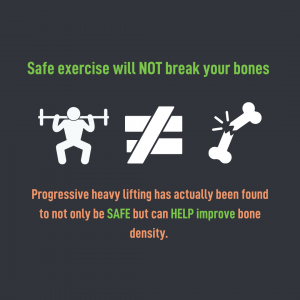
“I will break my bones if I exercise”
Exercise will not break your bones, it is safe and research shows it is effective at slowing the progression of the condition. Therefore by not exercising you are increasing your risk through physical inactivity.
“I was told that my bones are frail and more susceptible to fractures, therefore if I lift heavy things, I will break my bones?”
No, heavy lifting will not break your bones. Heavy lifting is a way to load the bones to prevent the decline in BMD. Not exercising will increase your risk of fractures more so than completing exercise.
What exercise specifically?
Exercise is like medicine. It is important to have the right type, dose, and frequency for a particular chronic health condition and individualized programming. General exercise is great, but it might not be the most effective at treating a given health concern or goals of an individual.
Type of exercise for Osteoporosis:
Dynamic load bearing exercises are required to stimulate the changes within the bone and muscles. Some exercises are not weight bearing OR do not have enough load going through the joints to stimulate osteogenic change. Evidence says that relatively high bone strain and for the force to be applied rapidly, is required to elicit an osteogenic response. Depending on your classification and T-Score different levels of loading is appropriate, and considerations should be put in place prior to completing high intensity loading. BUT moderate impact loading and high load progressive resistance training is SAFE for individuals with LOW bone mass. It is always best to talk to an AEP prior to commencing this type of exercise to ensure the correct exercises are prescribed.
Examples of load bearing exercises are:
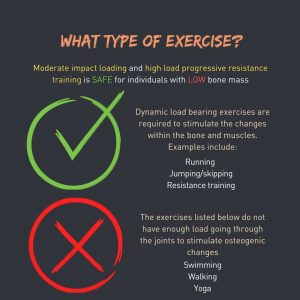
- Jumping
- Resistance training
- Running
- Skipping
Although swimming, walking and yoga are great types of exercise for GENERAL health benefits, they unfortunately do not provide the right stimulus for your bones and therefore can be completed and used but NOT as part of a prevention strategy for osteoporosis.
How much load is required to manage and prevent osteoporosis?
Moderate to high weight bearing loads greater than 2 times bodyweight are required in short bouts separated by rest.
How often do I need to compete exercise to manage and prevent osteoporosis?
10-50 repetitions a day 3 times a week. There are added benefits if it is completed more regularly 4-7 times a week.
Additional information:
Before starting an exercise program, is it best to have a chat with an Accredited Exercise Physiologist to see what type and dose of exercise is best for you. When an Exercise Physiologist is prescribing an exercise program for Osteoporosis they will incorporate elements of balance, dual tasking, muscular strength, and gait stability as well to decrease the risk of falls.
Written by: Emma Abfalter AEP, AES