Half of all Australians are currently living with at least one chronic illness, defined as any health condition lasting longer than 3 months [1]. This includes asthma, arthritis, cancer, chronic pain, diabetes, obesity, heart disease, mental health disorders and others.
That’s almost 13 million Australians living with conditions that may negatively impact their quality of life and put them at risk of further health consequences. Unsurprisingly, people with these conditions can be cautious when it comes to threats of injury and a worsening of their condition. There is a common belief among people with chronic diseases and those around them, that vigorous exercise may possess such a threat to their health. As a result, we often directly and indirectly encourage those with health concerns to avoid exertion and look after themselves through less active means.
It begs the question; what is more dangerous for someone with a chronic illness? Working hard or hardly working?
Most people with a chronic health condition know that being active is good for their health, though many are apprehensive about high intensity exercise. They may have concerns such as “isn’t it dangerous to get my heart rate up high?”, “Should someone my age be pushing themselves that hard?” or “I’m already fatigued, won’t that make it worse?”.
The answer is more encouraging than you might think.
Before we answer these questions we need to understand what high intensity exercise is and how it is generally conducted.
High Intensity Interval Training
If you’ve been around gyms or health clubs, chances are you’ve heard of the term high intensity interval training or ‘HIIT’ before. You might’ve heard people mention that they are doing HIIT workouts on YouTube or attending HIIT classes. What are they on about? and why are they always posting it on Instagram?
There’s a lot of interpretations of HIIT, but fundamentally it is a form of exercise that is composed of brief intense bouts, interspersed by periods of low intensity or complete rest. That’s it.
So those people throwing kettlebells around at the gym and doing burpees in their living room might be doing HIIT, but in reality, HIIT can involve any form of exercise. From boxing, to cycling, to swimming, the mode is irrelevant, which makes it highly adaptable and enjoyable.
We’ll get onto what really separates HIIT from other exercise a little later.
Where did HIIT come from?

Working vigorously in an intermittent fashion has likely been around long before the concept of HIIT emerged. However, the first appearance of any structured form of HIIT came about in the early 1900s. First implemented by champion Finnish track and field athletes, namely Hannes Kolehmainen, a 4-time Olympic gold medallist and world record holder, and Paavo Nurmi, the world’s most successful distance runner between 1920 and 1930, with 9 Olympic gold medals. “The Flying Finns” as they were known, were notorious for their speed and attributed much of their success to the use of high intensity interval training.
You might be wondering “I’m not training for the Olympics? Why do I care about what a few runners did over a century ago?”
Well, it seems that the same method the Finns used to run faster may also help us to age slower [2]. So, if you’re competing for the “Centenarian Olympics” [3], HIIT might just give you the competitive edge.
HIIT is trending, and for good reason.
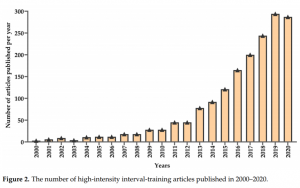
From the track to the clinic, what was once used as a performance enhancer for athletes is increasingly being used as a therapeutic tool to help those with chronic health conditions. This is thanks to the explosion of scientific research around HIIT over the last two decades [4], and the investigation into how this form of training affects our health.
Here are just a few promising examples from recent evidence, demonstrating the effectiveness of HIIT for improving health outcomes in those with various chronic diseases:
- Improves Cardiorespiratory fitness (one of the key determinants of health outcomes and quality of life) by almost double that of moderate intensity continuous training (MICT), in individuals with lifestyle-induced chronic diseases [5].
- Shown to be superior when compared to usual care for improving physical fitness and health-related outcomes in cancer survivors across all stages of therapy and aftercare [6].
- Improves multiple markers of Metabolic syndrome such as blood glucose, blood pressure and visceral adiposity [7].
- Effective in treating generalised anxiety and depressive disorders, equal to or greater than existing first line therapies such as cognitive behavioural therapy and antidepressants [8].
Why is HIIT so powerful?

There are many interesting mechanistic studies that detail the specific physiological effects of HIIT, but to delve into those would probably be more intense than the exercise itself.
To provide a little more depth, the following excerpts highlight the distinct effects of HIIT and MICT, and what features of HIIT may be underpinning the benefits we see:
“HIIT provides a robust stimulus for central adaptations and metabolic stress while MICT mainly triggers peripheral adaptations contributing to muscular oxygen extraction and metabolic efficiency” [3].
“Physiological adaptations are not only attributable to the intensity per se but also the intrinsic nature of intermittent exercise” [3].
Ok so it might have advantages, but won’t it be harder to stick to?
HIIT indeed requires more effort, more huffing and puffing.
However, it has been shown to elicit higher enjoyment than MICT [9] and has lower dropout rates than traditional exercise in previously sedentary individuals [10]. Maybe because it often takes about half the time!
Although you can make it torturous: “a single bout of HIIT at a too strenuous intensity with low rest results in decreased enjoyment” [10].
The benefits look promising, but how safe is it?
To answer the initial concerns:
Q: “Isn’t it dangerous to get my heart rate up high?”
A: HIIT improves cardiac function and has a low incidence of adverse cardiac events, similar to MICT [11].
Q: “Should someone my age be pushing themselves that hard?”
A: Older adults may experience a reversal in age-related deterioration of their muscle cells after engaging in HIIT, to a greater degree than younger individuals [2].
Q: “Won’t HIIT make my fatigue worse?”
A: HIIT doesn’t appear to increase fatigue more than MICT in individuals with chronic fatigue and can be considered in a graded exercise program [12].
Perhaps none of these scenarios relate to your circumstance. Fortunately, there is evidence for many other conditions:
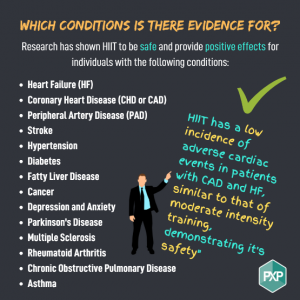
HIIT has even been shown to be safe in patients recently hospitalized with severe COVID-19! [13].
How do I do HIIT correctly?
So, we know it’s relatively safe and can provide a great deal of benefit to people with various health concerns.
Now let’s talk about how to do it properly.
All that HIIT requires is that you work at a high enough intensity, rest adequately and repeat.
So, what is high intensity?

Rating of Perceived Exertion or RPE is one of the best measures to monitor your intensity.
You want to use a 6 – 20 Borg scale where 6 is equivalent to ‘sitting down and resting’ and 20 is at an intensity you can only maintain for ‘5 to 20 seconds’ before being completely exhausted.
During the work periods you want to be working at or above a RPE of 15, this is where you can only talk in syllables and have heavy breathing.
Heart rate works well too
During the work periods you want to be > 75% of your heart rate max
To estimate your HRmax, take 220 and deduct your age.
So, if you’re 57, 220 – 57 = 163 is your HRmax.
75% of this or (163 x 0.75) is 122. Meaning your HR must exceed 122bpm to be considered high intensity.
*For some people HR may not be a good measure (e.g. those on betablockers), so use RPE instead.
The time of the work period will depend on the intensity. This can range from 20s – 4 minutes.
Alright, what about the rest periods?
Rest periods should generally be at a low intensity <13 RPE or completely passive (no active movement).
Rest periods generally last anywhere from 10 seconds – 4 minutes.
Your heart rate should generally drop <65% of your HRmax when resting, though the best indication of whether you’re recovering adequately in-between bouts is your ability to maintain the same output/effort during each bout.
If you find you can’t pedal/run/swim nowhere near as fast as the previous bout, then chances are the rest period needs to be extended or the intensity must come down slightly.
The number of bouts performed will often vary from 4 – 12. Performing more bouts as your fitness increases is another way to continue progressing.
Finally, it is best to ensure you warm up and cool down adequately for at least 5 minutes before and after the session.
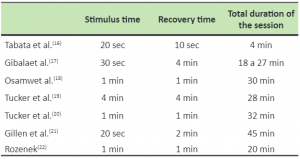
Example of HIIT protocols [14]
Caveats to HIIT
Don’t run before you can walk
- If you’re someone who isn’t used to moderate intensity cardio, it might be best to get accustomed to this before trying HIIT.
- Strength and neuromuscular coordination may be a prerequisite for impact type HIIT training to reduce injury risk (running, jumping etc.).
- Medical clearance from your GP before commencing HIIT is important as there are outright contraindications.
- Supervision by an accredited exercise physiologist may be needed for those at high risk.
If you’re still not sure on how to get started or if HIIT is right for you, an accredited exercise physiologist can give you the correct guidance on the right steps to take.
With any form of exercise there is a risk in doing and not doing. We know that the consequences of not exercising is having a much greater impact on our health and health system than that of too much exercise. With the influx of evidence supporting the efficacy and safety of HIIT in people with chronic illness, it seems we can shift away from conservative treatment and move towards greater outcomes through more advanced forms of exercise.
Written by: Chris Kardaras AEP, AES
References
- Chronic disease overview. Australian Institute of Health and Welfare. (n.d.). Retrieved September 12, 2021, from https://www.aihw.gov.au/reports-data/health-conditions-disability-deaths/chronic-disease/overview.
- Exercise – centenarian olympics archives. Peter Attia. (n.d.). Retrieved September 16, 2021, from https://peterattiamd.com/tag/exercise-centenarian-olympics/.
- Atakan, M. M., Li, Y., Koşar, Ş. N., Turnagöl, H. H., & Yan, X. (2021). Evidence-Based Effects of High-Intensity Interval Training on Exercise Capacity and Health: A Review with Historical Perspective. International Journal of Environmental Research and Public Health, 18(13), 7201.
- Robinson, M. M., Dasari, S., Konopka, A. R., Johnson, M. L., Manjunatha, S., Esponda, R. R., … & Nair, K. S. (2017). Enhanced protein translation underlies improved metabolic and physical adaptations to different exercise training modes in young and old humans. Cell metabolism, 25(3), 581-592.
- Weston, K. S., Wisløff, U., & Coombes, J. S. (2014). High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. British journal of sports medicine, 48(16), 1227-1234.
- Mugele, H., Freitag, N., Wilhelmi, J., Yang, Y., Cheng, S., Bloch, W., & Schumann, M. (2019). High-intensity interval training in the therapy and aftercare of cancer patients: a systematic review with meta-analysis. Journal of Cancer Survivorship, 13(2), 205-223.
- Serrablo-Torrejon, I., Lopez-Valenciano, A., Ayuso, M., Horton, E., Mayo, X., Medina-Gomez, G., … & Jimenez, A. (2020). High intensity interval training exercise-induced physiological changes and their potential influence on metabolic syndrome clinical biomarkers: a meta-analysis. BMC Endocrine Disorders, 20(1), 1-12.
- Plag, J., Schmidt-Hellinger, P., Klippstein, T., Mumm, J. L., Wolfarth, B., Petzold, M. B., & Ströhle, A. (2020). Working out the worries: A randomized controlled trial of high intensity interval training in generalized anxiety disorder. Journal of Anxiety Disorders, 76, 102311.
- Oliveira, B. R. R., Santos, T. M., Kilpatrick, M., Pires, F. O., & Deslandes, A. C. (2018). Affective and enjoyment responses in high intensity interval training and continuous training: A systematic review and meta-analysis. PloS one, 13(6), e0197124.
- Reljic, D., Lampe, D., Wolf, F., Zopf, Y., Herrmann, H. J., & Fischer, J. (2019). Prevalence and predictors of dropout from high‐intensity interval training in sedentary individuals: A meta‐analysis. Scandinavian journal of medicine & science in sports, 29(9), 1288-1304.
- Wewege, M. A., Ahn, D., Yu, J., Liou, K., & Keech, A. (2018). High‐intensity interval training for patients with cardiovascular disease—Is it safe? A systematic review. Journal of the American Heart Association, 7(21), e009305.
- Sandler, C. X., Lloyd, A. R., & Barry, B. K. (2016). Fatigue Exacerbation by Interval or Continuous Exercise in Chronic Fatigue Syndrome. Medicine and science in sports and exercise, 48(10), 1875-1885.
- Foged, F., Rasmussen, I. E., Budde, J. B., Rasmussen, R. S., Rasmussen, V., Lyngbæk, M., … & Christensen, R. H. (2021). Fidelity, tolerability and safety of acute high-intensity interval training after hospitalisation for COVID-19: a randomised cross-over trial. BMJ open sport & exercise medicine, 7(3), e001156.
- Machado, A. F., Nunes, R. D. A. M., de Souza Vale, R. G., Rica, R. L., Junior, A. F., & Bocalini, D. S. (2017). High intensity interval training with body weight: the new calisthenics?. Manual Therapy, Posturology & Rehabilitation Journal, 1-4.