What is POTS?
It is an acronym that stands for Postural Orthostatic Tachycardia Syndrome.
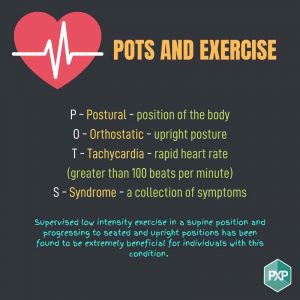
Postural – position of the body
Orthostatic – upright posture
Tachycardia – rapid heart rate greater than 100 beats per minute
Syndrome – a collection of symptoms
It is a condition where there is a dysregulation of the autonomic nervous system so the body systems that usually work automatically like pumping blood around our body or fighting infection don’t operate the way that they should. Majority of individuals with this condition are females aged between the ages of 15 and 50. The condition impacts a number of different body systems including our heart and blood composition, our immune system (cardiovascular, nervous, renal, immune and haematological) and our central nervous system or our fight, flight and freeze system. Postural Orthostatic Tachycardia Syndrome is a collection of symptoms that vary for individuals but the main sign is the rapid increase in heart rate after changing position from seated to standing without hypotension (drop in blood pressure). Each individual experiences the condition differently and the level of severity is quite varied.
Common symptoms include:
Fatigue, rapid heart rate (tachycardia), tremors, anxiety, dizziness, GI disturbances, vision changes and cognitive impairment/brain fog.
Conditions that often accompany POTS include:
- Hypermobility spectrum disorder or EDS Ehlers Danlos Syndrome
- Chronic fatigue Syndrome
- Chronic Pain
- Central Sensitisation
- Mast Cell Activation Disorder
Why is the body increasing heart rate with changes in positioning?
Usually when an individual stands upright or moves from sitting to standing the body is able to contract blood vessels, and slightly increase heart rate to pump the blood towards the heart and the brain preventing the blood pooling in your limbs, being dizzy or even passing out. In POTS these systems don’t work as well and the body rapidly increases their heart rate to ensure the blood gets to the brain and heart. The body is working quite hard to do these actions which is one of the reasons why an individual with this condition may then experience fatigue or Post-exertional malaise that does not correlate with the level of intensity of the activity.
How can exercise help?
Cardiovascular exercise
Cardiovascular de-conditioning is a major contributor to symptoms, if an individual has a higher capacity and is physically fitter their severity of symptoms is decreased. When your heart is conditioned it has a greater capacity to pump blood around your body. The heart is stronger so it contracts more forcefully pushing more blood out and doesn’t increase heart rate as rapidly during lower intensity exercise. Other systems such as the lungs, blood vessels and muscles also become more efficient enabling more oxygen to be transported and used.


Strength training
Muscles especially in the lower limbs when they contract it assists with pushing blood back to the heart. When the muscles are stronger it produces a larger pumping action pumping the blood back to the heart faster.
To begin strength training individuals with POTS are able to manage supine (laying down on back) exercises a lot easier than seated or standing exercises as the body does not have to work against gravity to pump the blood back to the heart and brain.
Supervised low intensity exercise in a supine position and progressing to seated and upright positions has been found to be extremely beneficial for individuals with this condition.


Other techniques to improve symptom management
- Adequate hydration
- Salt and electrolyte consumption
- Compression garments
- Pacing
- Cold drinks of water when experiencing symptoms
The best way to get started is to have a chat with an Accredited Exercise Physiologist and see where the best place is to start.
Written by: Emma Abfalter
References:
- Postural orthostatic tachycardia syndrome (POTS): State of the science and clinical care from a 2019 National Institutes of Health Expert Consensus Meeting https://reader.elsevier.com/reader/sd/pii/S1566070221000588?token=32975F01F24310626F68DFED43FCEEB566375E67BABDADEF2450926A0B794025968FC8817D88F520F3F0A0A1660264A1&originRegion=us-east-1&originCreation=20220721232920
- Skeletal muscle pump drives control of cardiovascular and postural systems: https://www.nature.com/articles/srep45301#:~:text=During%20upright%20posture%2C%20skeletal%20muscles,heart%20(skeletal%20muscle%20pump).
- POTS – Circulation AHA journal – https://www.ahajournals.org/doi/10.1161/circulationaha.112.144501
- Postural Orthostatic Tachycardia Syndrome https://www.ncbi.nlm.nih.gov/books/NBK541074/
- Exercise and non-pharmacological treatment of POTS https://www.autonomicneuroscience.com/action/showPdf?pii=S1566-0702%2818%2930066-3
- The face of postural tachycardia syndrome – insights from a large cross-sectional online community-based survey https://onlinelibrary.wiley.com/doi/10.1111/joim.12895
- The effect of water temperature on orthostatic tolerance: a randomised crossover trial https://link.springer.com/article/10.1007/s10286-022-00860-7
- POTS UK https://www.potsuk.org/about-pots/what-is-pots/