Review of the 2022 Consensus Statement on Concussion in Sport
Concussion and its detrimental impact is becoming an increasingly popular topic in both recreational and professional sport. Despite the additional attention, what does this mean for an individual and how can we best manage and improve an individual’s capacity to return to sport, school or work.
This article is focused on the 2022 publication of the latest guidelines for concussion management in sport. The article covers:
- Definition of concussion
- What symptoms to watch at the time of concussion
- Diagnosis
- Returning to sport/ learning
- What the strategies to ensure a successful return
- What are the current guidelines for retirement post concussion?
Official definition of Sports related concussion.
“Sport-related concussion is a traumatic brain injury caused by a direct blow to the head, neck or body, resulting in an impulsive force being transmitted to the brain that occurs in sports and exercise-related activities. This initiates a neurotransmitter and metabolic cascade, with possible axonal injury, blood flow change and inflammation affecting the brain.
Signs and symptoms may present immediately or evolve over minutes or hours, and commonly resolve within days but can be prolonged. No abnormality is seen on standard structural neuroimaging studies (i.e., computed tomography or magnetic resonance imaging T1- and T2-weighted images), but in the research setting, abnormalities may be present on functional, blood flow or metabolic imaging studies. Sport-related concussion results in a range of clinical symptoms and signs that may or may not involve loss of consciousness. The clinical symptoms and signs of concussion cannot be explained solely by (but may occur concomitantly with) drug, alcohol, or medication use, other injuries (such as cervical injuries, peripheral vestibular dysfunction) or other comorbidities (such as psychological factors or coexisting medical conditions).”
What can be done to prevent concussions occurring?
Prior to concussion, there are training strategies that current research suggests can decrease concussion rates. The training is neuromuscular training prior to the game/training, and should be completed 3 times a week. This particular paper looked at Rugby and found this training decreased rates of concussion in males by 59%. This theory needs to be tested and implemented with a greater target demographic to ensure that it also has applicability to other population groups (e.g., females, other sports).
At the time of concussion
The new consensus statement has updated the current assessment tool for concussion, it is now the “Sport Concussion Assessment Tool (SCAT 6)”. This is to be completed at the time of the concussion for up to 72 hours post for the best validity, but can be used for up to one week post-concussion. Current regulations state that the individual must be removed from the field if concussion is suspected. The following symptoms require staying off for the rest of the game rather than to return to playing during a game.
- Loss of consciousness
- Seizure
- Tonic posturing
- Ataxia
- Poor balance
- Confusion
- Behavioural changes
- Amnesia
The AFL guidelines mention a few additional signs and patient reported symptoms to look out for they include:
- Vomiting after a head knock
- Grabbing and clutching the head
- Dazed, vacant or black look
- Unsteady on feet or lack of coordination
- Headache
- Blurred vision
- Sensitivity to light and noise
- More irritable or emotional than usual
- Neck pain
- Difficulty concentrating
These symptoms may evolve over minutes, hours even days post event.
There is an app that can be used for concussion assessment called ‘Headcheck’ and this enables you to fill out on the spot, concussion check, obtain concussion recovery guidelines and also some additional information to understand more information surrounding concussions. This is not the same as a SCAT6 or CRT -6 therefore you will still need to go to the GP for an official diagnosis. If there is a suspected concussion the app will suggest that you visit the GP as soon as possible, but it will also give you some guidance in how to manage the concussion in the initial stages.

Diagnosis
Concussion recognition tool -6 (CRT-6) and (SCAT-6) and the child SCAT -6 best used in the first 72 hours (up to one week post injury). Cervicovestibular rehabilitation recommended for individuals with neck pain, headaches, Dizziness and balance problems. Persistent symptoms >4 weeks multimodal clinical assessment Limited evidence for athletes aged 5-12 years old and para athletes
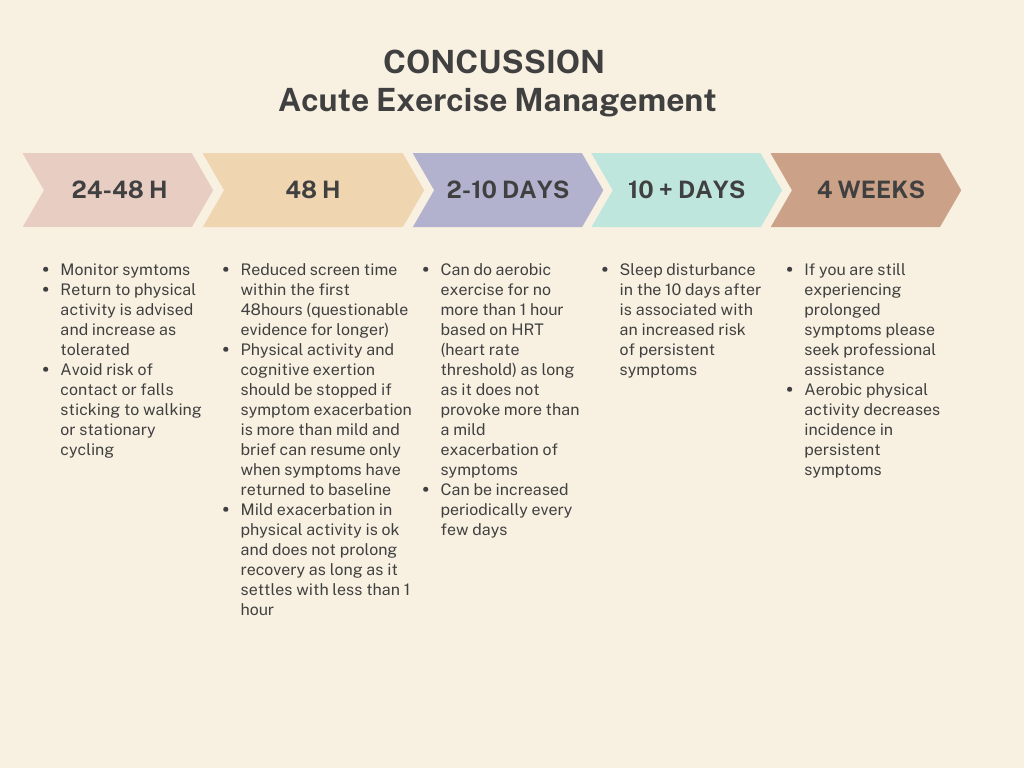
Acute exercise management and referral
With persistent symptoms (longer than 4 weeks) refer to a professional that has specialized knowledge in the following:
- Management of cervicogenic symptoms
- Migraine
- Headache
- Psychological disturbances
- Vestibular signs
- Oculo-motor manifestation
These professionals include GP’s, Neurological Physiotherapist, Vestibular physiotherapist, Psychologist and Exercise Physiologists. Rehabilitation required if the following symptoms are present >10 days post continued dizziness, neck pain and or headaches cervicovestibular rehab is recommended
Primary recovery measures
Three components:
- Symptom reports at rest, during exercise/ physical exertion and then cognitive tasks
- Outcome measures covering headaches, standing balance, dynamic balance,vestibulo-ocular reflex (VOR) function, oculomotor function (OM) symptom reproduction with VOR and OM, cognition and dual tasking
- Measures of return to learn/ return to sport
Definitions of recovery
1.Symptom resolution at rest
- No associated concussion symptoms at rest
2. Complete symptom resolution
- Resolution of symptoms associated with the concussion at rest and no on set of symptoms during or after maximal physical and cognitive exertion
3. Return to Learn
- Returning to primary pre learning activity no additional learning support (including school accommodations or learning adjustments
4. Return to Sport
- Completion of return to sport strategy with no symptoms and no clinical findings associated with the current concussion at rest and with maximum exertion
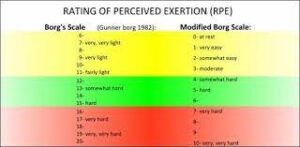
- Measuring maximum exertion can be a scale called Borg Rate of perceived exertion. It is a 6-20 or 0-10 scale and has explanations of what the numbers are equivalent with.
Return to learn recommendations
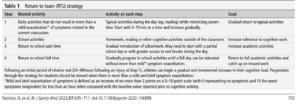
- 93% of individuals return to learning 10 days post with no issues
- To minimise disruption to learning the following guidelines are in place:
- Early return to activity should be encouraged provided that symptoms do not increase more than 2 points on the symptom severity scale 0-10 for less than an hour
- Environmental adjustments
- Modified attendance at school/ work, frequent rest breaks and limited screen time
- Physical adjustments
- Risk of contact and falls (contact sports)
- Curriculum/Testing adjustments
- Extra time to complete assignments and tasks
- Delaying tests or permitting additional time
- Progression to removing these adjustments are the same as prior can increase gradually as long as there is no increase in symptoms greater than 2 out of ten symptom severity scale and resolution of symptoms in less than 1 hour post activity.
Return to Sport
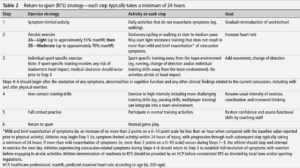
Able to begin symptom limited recovery 24 hours post, further progression typically takes a minimum of 24 hours. Usual recovery time minimum a week but full return to sport can take up to 1 month. Return to sport varies between individuals depending on symptom severity. Athletes that are struggling to recover after week 2-4 might benefit from additional assistance with rehabilitation from a multidisciplinary team. Medical determination/ clearance should occur prior to returning to at risk activities (collision, contact or falls)
Long term effects of Repeated Concussion
CTE-NC (Chronic Traumatic Encephalopathy-Neuropathological change) is a condition that is only diagnosable post mortem. CTE-NC is not a clinical diagnosis. The consensus criteria 2021 describes Traumatic Encephalopathy Syndrome, which is diagnosable condition when an individual is living and it is the collection of the following symptoms: There is further research being conducted that is looking into the severity of Traumatic Encephalopathy Syndrome and how it correlates with CTE-NC post mortem.
There is currently limited evidence on these conditions as there are a lot of factors to be considered. Current research suggests that the condition is very uncommon among community sporting individuals and more prevalent among former professional athletes with a high exposure to repetitive head trauma. At an amateur sporting level, currently the research is that there is no increased risk of depression or suicidal ideation during early adulthood or older adults. Professionally the research currently states that for former professional soccer players there is not an increased risk of psychiatric hospitalisation. Former professional football is not at an increased risk of death associated with having a psychiatric disorder.
Retirement Post Concussion
Individually sporting codes each have different medical regulations surrounding concussion and clearance to returning to sport or retiring. Currently, there are no overarching concussion guidelines across all sporting codes that state specific markers or factors which may force an individual to retire from sport. The current recommendations are that the decision is a multidisciplinary one that includes medical and health professionals, the individual involved and parents if they are under 18 years old. These individuals have to factor in evidence of injury, risk tolerance of the individual and the sport, and athletes preference (if they have the psychological readiness to make the decision). If the individual is a child, return to learning should also be considered and how it impacts the individual’s capacity to learn.
Despite mentioning retirement from the sport, this does not mean retiring from physical activity. Lower impact or non-contact sports have a decreased risk of concussion but can still meet an individual’s recreational, physical, and psychological needs.
*
Please take note that the above is for adults only. The current guidelines have restricted guidelines and recommendations for parra athletes and paediatric clients.
**
This is a summary of the Consensus statement on concussion in sport: the 6th International Conference on Concussion in Sport– Amsterdam, October 2022. You can find the full article here: https://bjsm.bmj.com/content/bjsports/57/11/695.full.pdf.
Additional resources
https://www.concussioninsport.gov.au/home
Written by: Emma Abfalter AEP & AES